 It seems I hit a nerve with my last post on “Why No Gels”. There is a nuance to be highlighted with regards to performance nutrition: the separation of fatigue due to a drop in blood volume and fatigue due to a lack of carbohydrate. This Part 2 will focus on the basic physiology to give insight on Part 1 (as well as some solutions!)
It seems I hit a nerve with my last post on “Why No Gels”. There is a nuance to be highlighted with regards to performance nutrition: the separation of fatigue due to a drop in blood volume and fatigue due to a lack of carbohydrate. This Part 2 will focus on the basic physiology to give insight on Part 1 (as well as some solutions!)
Open any exercise physiology textbook and the first factor of fatigue is a drop in blood volume, with the second factor of fatigue decreased carbohydrate availability. Why? Simplistically, you can rectify low circulating carbohydrate pretty effectively by eating something and feeling the effects within minutes. A drop in blood volume is more complex, and it takes hours to rectify (as it involves the kidney regulatory hormones aldosterone and arginine vasopressin).
Blood volume is the red cells and plasma in circulation. When discussing exercise and fluid shifts, the term “plasma volume” is often used, as this refers to the watery component of blood. With the onset of exercise, there is a shift of blood flow to supply the working muscles and to the skin, to divert the increased heat produced (from muscular contraction). With the increased demand for blood to the muscles and skin, there is hypoperfusion of other organs, including hypoperfusion of the GI system.
As exercise continues and plasma volume is lost through sweating, breathing, and gastrointestinal water usage, available circulating blood diminishes (there is less overall water in the blood, thus it is “thicker”). An endurance athlete will feel the drop in blood volume as “muscle fatigue”. As the viscosity of blood increases, the competition between the skin and muscles becomes fiercer; with the skin winning over muscle perfusion. Heat is a large threat to the body, the actual window of survival core temperature perturbation is quite narrow: 37-39.5°C (98.6-103.1ºF – Athletes often push themselves to a core temperature of 40°C before true adverse effects of heat stress are seen.). As heat storage of the body increases and more blood is shunted to the skin, there is less blood for muscle metabolism- nature’s purpose: shut down the threat. By this, I mean, less blood for muscle metabolism means fewer contractions, thus less heat produced (the temperate of the muscle itself contributes to fatigue as well by denaturing the contractile proteins). This is muscle fatigue – a drop in power. In a traditional mentality, this is when an athlete will typically reach for a gel or other quick hit of carbohydrate, thinking they are low in carbohydrate; but it is water deficit of the blood that forces the fatigue.
What impact does the drop in blood volume have on nutrient uptake? Plenty. The intestine is the primary organ for absorption of fluids, nutrients, and electrolytes. During prolonged exercise that increases core temperature, blood flow to the GI may be reduced by up to 80% to provide sufficient blood to the working muscles and skin. As core temperature approaches 39ºC, the intestinal temperature may be as high as 41ºC, leading to cell damage. In addition, the shunting of blood away from the intestines, hypoperfusion causes ischemia, leading to oxidative damage; both mechanisms compromise the integrity of the intestinal tract: from large-action motility to the small-action of epithelial cell tight junction permeability. The disruption to the tight junction proteins results in an increased release of luminal endotoxins (a.k.a bacteria) into the blood stream. These endotoxins increase systemic immune response (inflammation), oxidation, and perpetuates gastrointestinal dysfunction.
As an endurance athlete, you should be concerned with how to mitigate this drop in blood volume and reduced blood flow to the GI system; what you eat and drink plays a critical part on your overall performance (a.k.a. delay fatigue and maintain power) due to the effects on fluid dynamics.
Main factors which affect fluid absorption include: the composition of what you are drinking: (osmolality, carbohydrate choices, sodium content); gastric emptying (how fast a solution exits the stomach and enters the small intestines); hypo- vs hyper-osmotic changes in the intestinal lumen; and co-transport mechanisms.
Several additional articles can cover composition and gastric emptying; in this one, I want to focus on the osmotic changes in the intestinal lumen and co-transport mechanisms. From my initial post “Why Not Gels” I discussed the impact of fructose and maltodextrin on the osmotic changes in the intestinal lumen:
“The second factor is the carbohydrate matrix of the gel. Research does show that the combination of two sugars is much faster than one for promoting carbohydrate absorption. When fructose and glucose are ingested in combination (either as fructose plus glucose, or as sucrose) the mean oxidized amount of the mixed sugars is ~66%, as opposed to fructose at 29% (women) to 45% (men) and glucose at 58%. But the actual absorption rate of the sugars is the contention here: glucose is absorbed from the intestine into the plasma via more than one active glucose co-transporter protein; reducing the contact time with the gut lumen. Fructose, however, is less efficient and slower to be absorbed due to less active transport mechanisms; leading to increased contact time with the gut lumen. Why is contact time significant? With incomplete and slow absorption, fructose produces a hyperosmolar environment in the intestines. What this means is that there is more solute than water, causing an increased pressure, signaling fluid to be drawn into the intestines, producing the known feelings of bloating, gas, diarrhea, and general GI discomfort.
Maltodextrin, a polysaccharide with the building blocks of glucose, is used in gels instead of straight glucose for several reasons. The primary rationale that maltodextrin does not affect osmolality as significantly as glucose, fructose or dextrose. Because maltodextrin is a long chain of glucose molecules, it doesn’t add as much to the number of solutes in a solution, thus a solution (gel or sports drink) can contain quite a bit of maltodextrin and still have a faster gastric emptying rate. From a carbohydrate availability standpoint, this is appealing as resultant glucose molecules are absorbed through the several glucose co-transporter proteins. Here is the caveat: because maltodextrin is a long chain of several glucose molecules, it is not completely hydrolyzed in the stomach; but continues in the small intestines where most of the hydrolysis takes place. In the small intestines, these multi-chain glucose molecules create the same hyperosmolar environment in the intestines as fructose.” (addendum: In the Rebuttal posted on Monday, there was a discussion of the science quoted for this particular statement. In ” Gisolfi, C, Lambert G, and Summers, R. Intestinal fluid absorption during exercise: role of sport drink osmolality and [Na]. Med. Sci. Sports Exerc. , Vol. 33, No. 6, 2001, pp. 907–915.” the authors specifically state “Although this beverage was hypotonic, which would promote the osmotic absorption of water, the hydrolysis of maltodextrin elevated luminal osmolality and slowed this process.” Moreover, it is critical to remember that there are two key sections for water and carbohydrate absorption in the intestines: the upper 25cm called the duodenum [the highly permeable segment responsible for bringing the chyme of the stomach to isotoncity] and the jejunum, the area of the small intestines most studied for carbohydrate and fluid absorption. In this article I am discussing the jejunum, where the effect of osmolality, sodium content, and type of carbohydrate has specific influence on water absorption rates.)
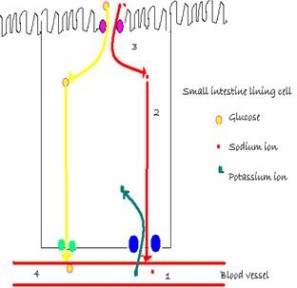
The sodium-glucose co-transport mechanism is critical for FLUID and glucose absorption across the cell membranes. Glucose is absorbed by the small intestine using an active process. Initially, the glucose and fluid exits the intestinal lumen via the sodium-glucose cotransporter protein, and is facilitated through an additional protein “gate”: GLUT-2. With the glucose, water and sodium also enter the blood; contributing to blood volume.
How does this affect you, the endurance athlete, in more practical terms? I’ll reiterate that to delay fatigue, you should implement nutritional strategies to promote blood volume maintenance. Why? Because with the reduction of blood volume, you effectively reduce your muscular power potential. In your nutrition strategy, you should look to avoid nutritional products which pull water OUT OF the blood, as this perpetuates the drop in blood volume.
If, by physiological logic, gels and other fructose-maltodextrin solutions, pull water out of circulation, then what should you eat to 1) reduce the impact on blood volume and 2) address your blood sugar needs (aka carbohydrate intake)? Real food. Yes, you can eat and ride. Your performance will improve with the separation of hydration from fueling. Suggestions/strategies: For a mountain biker, reading the course and doing things like eating AFTER the feed zone (get through the craziness first), then know where the base of a technical climb is- have a salted potato bite or a protein bite or energy chew or even a glucose tablet right there for a boost before the intensity; on the descent, drink some fluid; switchy single track? Same thing- know the course, plan your eating strategies according to the course profile, not time on the clock. You’re aiming for 3-4 FOOD calories per kg of body weight per hour (not a massive amount of calories – roughly 217 to 291 calories for a 160lb person). What about roadies? It’s slightly easier for you as the technical aspects are a wee bit less than the switchy singletrack of a mountain bike race. Try sandwich bites, “salty balls”, energy chews, and in the last hour of a ride or race when all that matters is keeping blood sugar UP for pace, use glucose tablets (they start to be absorbed in the mouth).
I challenge you to the hydration-power test: Use pee sticks and monitor your hydration. On days that you actually stay within a urine specific gravity (USg) of 1.015-1.025 you will find your power decline is less and your recovery is better. Where to get pee sticks? Amazon of course (Rapid Response with USg).
Final Words: I am a physiologist and nutrition scientist with a long professional research and sporting career; with a side project of a functional hydration company. The products of this company stem from my years an athlete suffering from dehydration and fueling issues (as well as my teammates), and the athletes and coaches I help with regards to environmental exercise physiology and nutrition; the advantage that I have had and still have, is that while I was suffering and trying to figure out what was going on, I had the availability to go to the lab to do the research on physiology of fluid balance, nutrition and heat stress during exercise. The articles I am writing for BikeRumor are to present the science of physiology, not to promote or “bash” any particular product; hence the recommended reading (below) and direction to the literature and lack of any product push.
 Stacy Sims, MSc, PhD, served as an exercise physiologist and nutrition scientist at Stanford University specializing in recovery and nutritional adaptations for health, body composition, and maximizing performance. During the past decade she has worked as an environmental physiologist and nutrition specialist for top professional cyclists and triathletes, ultra-endurance athletes, the Garmin/Slipstream Pro Cycling Team, USA Cycling Olympic Team (BMX and women’s track cycling), Team Tibco, Flying Lizard Motorsports, and Team Leopard-Trek, among others. She competes as a Cat 1 road cyclist and elite XTerra triathlete and is co-founder of OSMO Nutrition.
Stacy Sims, MSc, PhD, served as an exercise physiologist and nutrition scientist at Stanford University specializing in recovery and nutritional adaptations for health, body composition, and maximizing performance. During the past decade she has worked as an environmental physiologist and nutrition specialist for top professional cyclists and triathletes, ultra-endurance athletes, the Garmin/Slipstream Pro Cycling Team, USA Cycling Olympic Team (BMX and women’s track cycling), Team Tibco, Flying Lizard Motorsports, and Team Leopard-Trek, among others. She competes as a Cat 1 road cyclist and elite XTerra triathlete and is co-founder of OSMO Nutrition.
Recommended Reading:
- Mundel T. Exercise Heat Stress and Metabolism. Thermoregulation and Human Performance. Physiological and Biological Aspects. Med Sport Sci. 2008; 53:121-129.
- Zuhl M, Schneider S, Lanphere K, Conn C et al. Exercise Regulation of intestinal tight junction proteins. Br J Sports Med, 2014; 48:98-986.
- Van Wijck K, Lenaerts K, Grootjan J et al. Physiology and pathophysiology of splanchnic hypoperfusion and intestinal injury during exercise: strategies for evaluation and prevention; Am J Physiol Gastrointest Liver Physiol 2012; 303:G155-G168.
- Gisolfi, C, Lambert G, and Summers, R. Intestinal fluid absorption during exercise: role of sport drink osmolality and [Na]. Med. Sci. Sports Exerc. , Vol. 33, No. 6, 2001, pp. 907–915
- Sims, ST, L vanVliet, JD Cotter, and NJ Rehrer. “Sodium loading aids fluid balance and reduces physiological strain of trained men exercising in the heat.” Medicine and Sciences in Sports and Exercise, 39 (1), 123-130, 2007.
- Sims, ST, NJ Rehrer, ML Bell, and JD Cotter. “Pre-exercise sodium loading aids fluid balance and endurance for women exercising in the heat”, Journal of Applied Physiology, 103, 534-541, 2007.