In our high stressed, fast moving lives, we are often overtired, overstressed, undernourished (although overfed), and immunocompromised. This combination has far reaches (beyond the-wanting-to-sleep-at-work feeling) that extend to the interruption of our symbiosis with our gut bacteria.
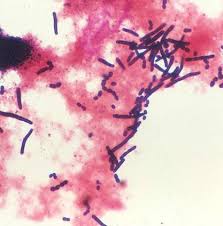
Um.. What? The human intestines contain ~100 trillion microbes (ten times more than any other cells in the body) comprised within four major phyla of bacteria: the Firmicutes, Bacteriodetes, Actinobacteria, and Proteobacteria. These microbes are under selective pressure to manipulate our eating behaviors and moods to increase their well-being; often at the expense of our overall health.
How does this come across in everyday habits? The struggle to resist certain cravings for foods that are high in sugar and fat (late night chocolate or almond butter anyone…) and increased inexplicable anxiety may be your gut flora sending messages, not a lack of “self control” or “freaking out”. The individual members of the microbiota have been shown to be highly dependent on the nutrient makeup of the diet. For example, Bifidobacteria grows well with a diet high in fiber, whereas Bacteriodetes does well with fat. In a comparison of the gut microbiota of obese to lean individuals there is a higher percentage of Firmicutes with a significantly lower percentage of Bacteriodetes, after a year-long dietary intervention, there was a significant increase in the Bacteriodetes (with a corresponding decrease in Firmicutes) and a signficant correlation to the percentage of fat mass lost with the rise in the percentage of the Baceriodetes.1
Stress and anxiety? These, too, are manipulated by microbes: In a double blind, randomized, placebo controlled trial, mood was significantly improved by drinking a probiotic containing Lactobacillius casei; with Lactobacillus helveticus and Bifidobacterum longus alleviating psychological distress5. And pain perception? Fasting increases the sensation and perception of pain due to proteins of the bacteria activating pain receptors (in response to a low concentration of growth-stimulating nutrients)6.
How and why can microbes in the gut affect such significant physiological and psychological aspects of ourselves?
One way the microbes manipulate your eating behaviour is to alter your cravings and preferences through changing receptor expression. For example, individuals who have a greater preference for fat had a different microbiome make up (a greater prevalence of Bacteroidetes) from those who preferred more sweets (greater prevalence of Prevotella). It is thought that the metabolites of these specific bacteria alter taste receptor expression to increase the consumption of nutrients which promote their growth.2,7
A more powerful way the gut microbiome controls eating behaviours and cravings is through neural feedback. The vagus nerve (the tenth cranial nerve that innervates the cardiac and digestive systems) is highly reactive to the presence of specific bacteria and bacterial metabolites (primarily the chemicals produced by the bacteria). How does this relate to food cravings and body weight? The vagus nerve regulates eating behaviour and body weight; thus overstimulation of the vagus nerve contributes to overeating; whereas increased parasympathetic outflow (think: calming relaxation, feel-good stimuli) improves the accuracy of food intake to energy expenditure.
How to manipulate your microbiome to work for you?
Over this past year I’ve worked with quite a few athletes (age group and professional) who have been battling undue fatigue, anxiety, GI issues, and overwhelming cravings. Lab results in all these athletes came back in the “normal” range, but they still struggled with these aforementioned issues regardless of rest or other interventions. Understanding how different strains of gut bacteria affect physiological and psychological outcomes, individualized plans to “reset” their gut flora alleviated the issues completely.
The easiest way to manipulate the gut flora is by the use of probiotics. Probiotics come in many different forms: tablets, pills/capsules, powders, yogurt/dairy drinks. Knowing what strains of bacteria to look for to help with specific symptoms is a bit tricky; but worth the time. For example, individuals who are stress-prone (anxious, poor sleep, high heart rate) with sweet-fat cravings have been shown to be low in the Lactobacilli strain, in particular L.casei, L.helevticus, and bifidobacterium longum. By treating the gut with probiotics, this can decrease the effect on the vagus nerve, reducing stress-related responses and sweet-fat cravings. The probiotic brand I most recommend is the Ultimate Flora (and often the Critical Care line of the brand). This one has a wide spectrum of the Lactobacilli and Bifidobacterium that work symbiotically whereas other OTC brands just include the traditional Lactobacillus acidophilus and/or bifidobacterium longus.
 Stacy Sims, MSc, PhD, served as an exercise physiologist and nutrition scientist at Stanford University specializing in recovery and nutritional adaptations for health, body composition, and maximizing performance. During the past decade she has worked as an environmental physiologist and nutrition specialist for top professional cyclists and triathletes, ultra-endurance athletes, the Garmin/Slipstream Pro Cycling Team, USA Cycling Olympic Team (BMX and women’s track cycling), Team Tibco, Flying Lizard Motorsports, and Team Leopard-Trek, among others. She competes as a Cat 1 road cyclist and elite XTerra triathlete and is co-founder of OSMO Nutrition.
Stacy Sims, MSc, PhD, served as an exercise physiologist and nutrition scientist at Stanford University specializing in recovery and nutritional adaptations for health, body composition, and maximizing performance. During the past decade she has worked as an environmental physiologist and nutrition specialist for top professional cyclists and triathletes, ultra-endurance athletes, the Garmin/Slipstream Pro Cycling Team, USA Cycling Olympic Team (BMX and women’s track cycling), Team Tibco, Flying Lizard Motorsports, and Team Leopard-Trek, among others. She competes as a Cat 1 road cyclist and elite XTerra triathlete and is co-founder of OSMO Nutrition.
Additional Reading:
1. Kocelak P, Zak-Gol A, Zahorska-Markiewicz et al. Resting energy expenditure and gut microbiota in obese and normal weight subjects. Eur Rev Med Pharmacol Sci 2013;17:2816-2821
2. Alcock J, Maley CC, Aktipis C.A. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays 2014; 36:71-81.
3. Khanna S, Tosh PK. A clinician’s primer on the role of microbiome in human health and disease. Mayo Clin Proc. 2014;89:107-114.
4. Rezzi S, Ramadan Z, Martin FP, Fay LB, et al. 2007. Human metabolic phenotypes link directly to specific dietary preferences in healthy individuals. J Proteome Res6: 4469–77.
5. Messaoudi M, Lalonde R, Violle N, Javelot H, et al. 2011. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br J Nutr105: 755–64.
6. Chiu IM, Heesters BA, Ghasemlou N, Von Hehn CA, et al. 2013. Bacteria activate sensory neurons that modulate pain and inflammation. Nature501: 52–7.
7. Clarke G, Stilling RM, Kennedy PJ, Stanton C, et al. 2014. Gut microbiota: the neglected endocrine organ. Mol Endocrinol (me2014:1108).